Granulocytes are the white blood cells that have small granules that contain proteins. The specific granulocytes are: neutrophilis, eosinophils, and basophilis [1,2].
- Granulocytes come from stem cells in the bone marrow of a person. The process of differentiation of these stems from the pluripotent hematopoietic stem cell to granulocytes is called granulopoiesis.
- Immature granulocytes are part of the immune system which responds to infection or inflammation. Immature granulocytes are an indication of an early stage of an infection.
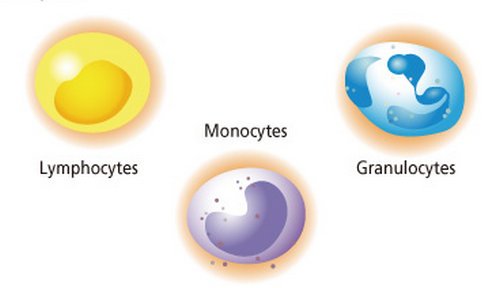
Types of leucocytes
What are immature granulocytes
- Immature granulocytes are white blood cells which only appear when the bone marrow is activated to fight of an infection they not only circulate blood but even if a healthy individual has a small count there should be no cause off concern when immature granulocytes. When absolute number of immature granulocyte increase significantly, this is a sign of infection [3,5,6].
- The neutrophil portion of the blood count usually goes upon when the immature granulocytes high levels begin to appear. This is a clue that there is something going on in the body such as bacterial infection, inflammatory disease, trauma in the body, use of steroids or maybe cancerous conditions.
- The elderly and young infants experience increase in immature granulocytes without neutrophils increase. [1]
- In the event this happens the increase needs to be thoroughly investigated.
Immature granulocyte count
- Apart from blood from neonates or pregnant women immature granulocytes appearance in the peripheral blood indicates an early stage response of an infection and inflammation or other stimuli of the bone marrow [4].
- Areas of research on the diagnostic importance of circulating immature granulocytes are focused on early, rapid discrimination of bacteria from infections that are viral particularly in the young children hence recognizing bacterial infection in neonates, and early bacterial recognition.[2, 3]
- For better understanding of how to get accurate immature granulocyte count we need to understand the differential blood count
- Differential gives relevant percentage of each type of white blood cells and also helps to reveal abnormal white blood cell population.
- Differential blood count could be performed using the following two methods.
- Automated differential blood counts: Automated hematology instruments that use multiple methods and parameters used to count and identify five major types of white blood cells in blood.
- Manual differential blood count: Manual count is done by visual examination of sample peripheral blood smear.
- Automated differential blood count consumes less time and costs less than routine blood smear examination. The automated technique allows thousands of the white blood cells to be examined. Visual examination can only allow 100-200 white blood cells to be examined. [4]
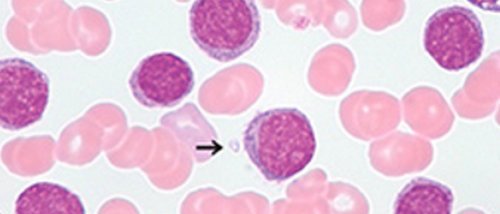
Cell images
Propose of preferential blood count
- Blood differential test measures the percentage of each white blood cell that individuals have in the blood. It also determines if there are any abnormalities or immature cells
Normal range
- The normal range describes where 95% of most health people population will lie.[5]
- It is very useful for biomedical scientists and haematology clinicians to have appropriate clinical details added to the request so that interpretation and best clinical advice can be given on the report where appropriate [7].
- A person diagnosed with CML should have routine blood tests which include complete blood count (CBC), blood differential and liver functioning tests which are done on a regular basis so as to help monitor treatment response.
- A complete blood count (CBC) which measures the number of white blood cells and platelets in a patient’s blood sample should be routinely monitored in CML patients.[6, 7]
Neutrophils
- These are a type of white blood cells involved in fighting infection. It’s of importance that they remain at adequate levels. As with platelets, neutrophils levels may be depressed in patients on myelosuppressive therapy such as imanitibbmesylate the normal range of the percentage of neutrophils is between 45-70% [9]
- More important than the neutrophils percentage is the absolute neutrophil count. Which will fall between 1.0-8.0 k/ul.
- The reason the absolute neutrophil count (ANC) represents the clear clinical picture better than the percentage of neutrophils is that, in cases where blood counts are suppressed by the therapy, percentage of neutrophils are higher when overall counts are law. One can calculate the ANC by multiplying the percentage of neutrophils by the percentage of bands by the total number of white blood cells, the number of white bands is usually quite low or zero.[8, 9]
Basophils
- The basophils should remain within the normal range generally between zero-two percent.
- Some medics believe that the absolute basophil count is of more importance than the basophils percentage and should fall between 0-0.3k/ul.
When low counts are of concern
- This depends on some individuals, the larger clinical picture and the therapy receive. In general for patients on imatianib mesylate therapy, a disease in those may be warranted by the following levels: the WBC less than 1.0k/ul; platelets less than 50k/ul;haemoglobin less than 10.0gm/Dl;and ANC less than 1.0k/ul.
Performance of blood differentials and CBCs
- All patients taking IM should have their blood counts monitored closely. Complete CBCs should be monitored closely on weekly intervals in chronic phase patients during first the first month of IM treatment.
- If counts are stable monitoring may occur monthly or even longer if appropriate. Patients in accelerating or blast crisis should have CBCs performed more often
Interpretation of full blood count
- A full blood count should be interpreted with reference to the clinical picture and other pathology results. Cautions must be given to certain abnormal results such as low platelets that may be artefact and rapids should be considered the laboratory will usually be investigate the abnormalities that may be haemotological in nature may accessing the blood film, the event of serious abnormalities that require agent attention such as acute leukemia, and severe hemolysis, the laboratory staff will alert the on-call haemotolic doctors.
Patients’ characteristics
- Patients whose age ranged between 19-88 years and their median ICU length of stay ranged 3-64 days were enrolled in a study to characterize disease severity the SAPs score was determined on the day of ICU admission the population had a median score of 37 showing expected ICU mortality rate of 19%.[10]
References:
- Sysmex-europe.com. Immature Granulocyte (IG) count – Sysmex Europe GmbH [Internet]. 2016 [cited 16 January 2016]. Available from: http://www.sysmex-europe.com/academy/knowledge-centre/sysmex-parameters/immature-granulocyte-ig-count.html
- Enkivillage.com. When Is Immature Granulocytes Too High and What Causes It? – EnkiVillage [Internet]. 2016 [cited 16 January 2016]. Available from: http://www.enkivillage.com/immature-granulocytes.html
- Healthline. Granulocytosis [Internet]. 2016 [cited 16 January 2016]. Available from: http://www.healthline.com/health/granulocytosis
- Nierhaus A, Klatte S, Linssen J, Eismann N, Wichmann D, Hedke J et al. Revisiting the white blood cell count: immature granulocytes count as a diagnostic marker to discriminate between SIRS and sepsis – a prospective, observational study. BMC Immunol. 2013;14(1):8.
- Clinlabnavigator.com. Immature granulocytes replaced bands as an indicator of infection | ClinLab Navigator [Internet]. 2016 [cited 16 January 2016]. Available from: http://www.clinlabnavigator.com/immature-granulocytes.html
- pdrhealth. Leukemia Diagnosis – Diseases and Conditions – PDR Health [Internet]. 2016 [cited 16 January 2016]. Available from: http://www.pdrhealth.com/diseases/leukemia/diagnosis
- Che Y, Shen D, Zhang S, Qi J. Identification of immature granulocytes in cancer chemotherapy patients by cell counting vs. microscopic examination of blood smears. Molecular and Clinical Oncology [Internet]. 2014 [cited 16 January 2016];2(2):207-211. Available from: http://www.spandidos-publications.com/mco/2/2/207
- Emedicine.medscape.com. Differential Blood Count: Reference Range, Interpretation, Collection and Panels [Internet]. 2016 [cited 16 January 2016]. Available from: http://emedicine.medscape.com/article/2085133-overview#showall
- Senthilnayagam B, Kumar T, Sukumaran J, M. J, Rao K. R. Automated Measurement of Immature Granulocytes: Performance Characteristics and Utility in Routine Clinical Practice. Pathology Research International. 2012;2012:1-6.
- HealthTap. Top 11 Doctor Insights on what does high immature granulocytes mean – HealthTap [Internet]. 2016 [cited 16 January 2016]. Available from: https://www.healthtap.com/topics/what-does-high-immature-granulocytes-mean
