Necrotizing Fasciitis
What is Necrotizing Fasciitis?
Necrotizing fasciitis, which is popular among layman’s term as a flesh-eating disease, is an infection caused by several bacteria affecting the fascia. The fascia is the fibrous connective membrane of the body, which may be separated from other specifically organized structures. Despite being called as the flesh-eating disease, the bacteria is not actually eating nor consuming the affected tissue.
In fact, it is the toxins released by the bacteria that result to the destruction of the affected tissue. The release of these toxins would also initiate the activation of T-cells that could result to excessive cytokine production and eventually lead to toxic shock syndrome. The toxic shock syndrome would usually be the fatal outcome once the bacteria’s toxins have infested on the tissues thereby affecting the blood flow to the body eventually.
Causes of Necrotizing Fasciitis
Necrotizing fasciitis can affect a person’s skin, fat and the surrounding tissues of a muscle. It is a rare condition but can be very progressive once an infection settles in. There are various bacteria that can cause the necrosis or death of the tissue. These bacterial invasions are classified into two types: Type I, which is a polymicrobial infection and Type II or monomicrobial infection.
- In Type 1 necrotizing fasciitis, the most common bacteria are the Aeromonashydrophila, Bacteroidesfragilis, Group A Streptococcus, Clostridium perfringens and Staphylococcus aureus.
- In Type II or monomicrobial infection, the causative organism could be any of the above mentioned bacteria. But the most common source of infection would be the Group A Streptococcus.
- Methilicilin Resistant Staphylococcus aureus (MRSA) is another type of microorganism that is highly likely to cause Type II necrotizing fasciitis.
Who are at high risks for necrotizing fasciitis?
- Persons who are the highest risks for this condition are those who are immunocompromised and those who have chronic conditions like diabetes, cancer, liver and kidney diseases.
- Persons with an open wound could also be infected as the wound could serve as a portal of entry for the microorganism especially if the person is exposed to sea water. The most common and the most dangerous affected parts are the abdominal wall, arms and the legs.
- Persons who have undergone surgery are also at risk because of the wounds obtained from surgery.
Signs and Symptoms
- Individuals who are affected by this condition would usually complain of severe pain.
- The affected tissue can also appear red and swollen and may feel hot upon touching.
- Fevers and chills can also be experienced as part of the inflammation process. These symptoms are actually similar to that of cellulitis.
- However, as the condition worsens, skin changes would continue to progress and would eventually include ulceration, formation of bullae, gas formation in the affected part and pus production. Worsening of the affected area can be quite fast, especially if not treated correctly either through surgery or antibiotics. Skin ulceration can progress to as fast as a few hours until such time it leads to tissue death or necrosis if not properly addressed.
- Other symptoms of the disease can include diarrhea and vomiting, as well as nausea, dizziness and weakness.
- Septic shock would be usually one of the most fatal outcomes that could result from necrotizing fasciitis. If left totally untreated, mortality rates could reach to as much as 73%.
Pictures
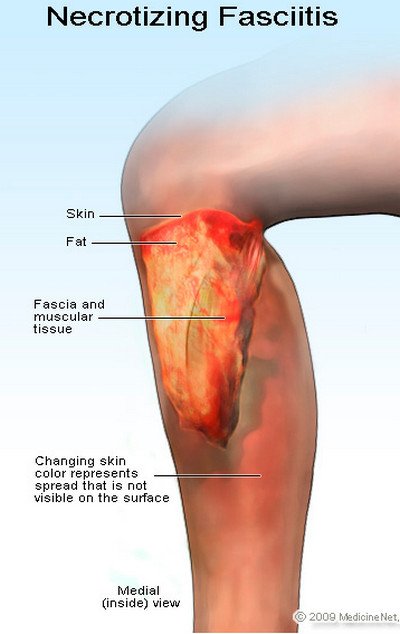
Picture 1: Necrotizing Fasciitis Features
Image source : Medicine Net
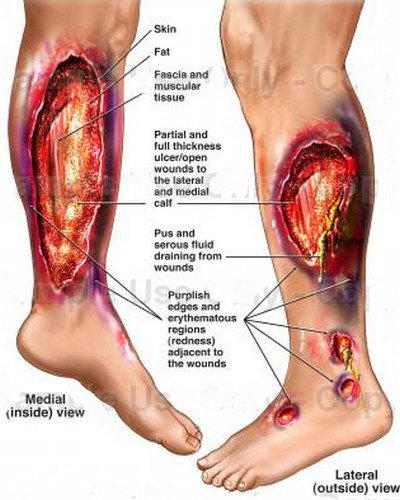
Picture 2: Necrotizing Fasciitis Picture
Image source : effguide

Necrotizing Fasciitis Diagnosis
There are several ways to diagnose necrotizing fasciitis.
- A physician or medical practitioner would usually start assessment based on a patient’s symptoms as well as the precipitating and predisposing factors that resulted to the condition. An interview regarding past surgeries or even exposure to seawater may predispose a patient to necrotizing fasciitis.
- In addition, a physical checkup of the affected area would affirm the physician’s suspicions regarding the disease.
- Once established, the physician could confirm the possibility and existence of the condition through different blood tests as well as CT scans and skin biopsy.
- Another more profound diagnosis tool would be through the use of the Laboratory Risk Indicator for Necrotizing Fasciitis (LRINEC) score. It uses a number of diagnostic tools to establish a positive result for necrotizing fasciitis. Greater than normal values for C-reactive protein, white blood cell count, creatinine, hemoglobin, and glucose plus an additional lower valuefor sodium would affirm a positive score for necrotizing fasciitis.
Treatment
- Initial treatment for the condition would usually involve a broad spectrum set of antibiotics as waiting for a confirmatory diagnosis would delay treatment and possibly increase the risk of morbidity and mortality.
- However, the preferred mode of treatment would still be surgical intervention. Patients with necrotizing fasciitis would require debridement 24 to 36 hours after the initial debridement and concurrently after so as to ensure complete cleansing of the entire wound takes place.
- Once the causative factor is identified through Gram staining, appropriate antimicrobial therapy could be initiated. For Gram positive cocci, penicillin, clindamycin and ampicillin sulbactam are the drugs of choice. Meanwhile, piperacillin-tazobactam, imipenem-cilastatin, meropenem, ertapenem, cefotazime are the preferred drugs for Gram negative microorganisms. Ampicillin sulbactam could also be utilized for Gram negative bacteria.
Note that any kind of treatment should be done by a medical professional.
Prognosis and Possible Complications
Necrotizing fasciitis if left untreated or treated wrongly could have a poor prognosis. Although a rare condition, it can progress quite fast. Diagnosis and treatment should therefore be prompt to give the affected person a better chance. Necrotizing fasciitis could result to the admission of a patient to an intensive care unit.
Death could be the worst complication brought about by the condition. Other complications, which could also result, include the loss of an organ and tissue damage through debridement and sometimes, even through amputation.
It is therefore important that once necrotizing fasciitis is suspected, it should be promptly referred to a physician so that immediate treatment may be given. The delay in treatment of the condition could turn out a fatal and disastrous outcome for the patient.
References:
http://en.wikipedia.org/wiki/Necrotizing_fasciitis
http://www.medicinenet.com/necrotizing_fasciitis/article.htm
http://www.webmd.com/a-to-z-guides/necrotizing-fasciitis-flesh-eating-bacteria-topic-overview