White Spots on the Lips
White spots on the lips can be a harmless or a symptom of a harmful illness. However, the lips are some of the most important parts cosmetically and are some of the most noticeable aspects of a person.
As such, persons with white spots on the lips tend to be self-conscious and the spots could lower their self-esteem, whether the spots are harmful or not [1].
The spots differ in appearance and morphology.
The differences serve as a basis for differentiating them and diagnosing the illnesses of which they are a symptom, if any.
Some are painful and others painless.

Image 1: An example of a white spot (Canker sores)
Picture Source: Wikipedia
Common Locations of the White Spots
- Areas around the lips
- Inside the lips
- Corners of the lips
- Vermilion border
- Upper lip
- Lower lip
- Some are not specific to the lips and may be found on other parts of the body [1]
Causes of White Spots on the Lips
Presence of White spots on lips can be due to:
- Illnesses
- Genetics
- Side effects of products used
- Low levels of personal hygiene [1]
Fordyce Spots
- Also referred to as Fordyce granules or sebaceous prominence
- Fordyce spots are small in size, their color ranges from white to yellowish, and are pimple-like.
- They are commonly found on the oral mucosa and the vermilion border – The sharp demarcation between the normal body skin and the red-colored region the lips [2]. They colonize both upper and lower lips.
- They are not specific to the lips and may be found on the inner surface of cheeks, tonsils, labia, penis, or scrotum. They appear on a sebaceous gland that lacks hair follicle [3].

Picture 2 : Fordyce spots
Image Source : fordycespotsforum.com
- Fordyce spots are not attributed to medical condition.
- They are painless and harmless.
- Should not be taken as a sign of sexually transmitted infection or cancer
- Affect both genders
- Tend to be larger with age
Treatment of Fordyce spots
- Electro desiccation
- Micro-punch technique
- Pulsed dye lasers
- Anti-sebum creams or ointments
- Chemical peels
- However, doctors discourage treating Fordyce spots
White spots due to Human Papilloma virus infection – HPV
- White spots on the lips could also be caused by HPV infection.
- Some of the strains of HPV are associated with various types of cancer e.g. vaginal, cervical, anal, mouth and oropharyngeal cancers.
- HPV can be transmitted via intimate skin-to-skin contact such as: anal, vaginal, or oral sex with an infected person [1].
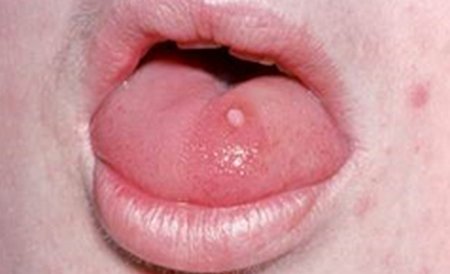
Photo 3 : Lip warts caused by HPV
Image Source : www.clinicaladvisor.com
- Warts due to oral HPV occur on the lips or anywhere inside the oral cavity.
- The spots are white in color, dome or flat –shaped and may appear as small, spiked projections.
- Painless unless irritated
Treatment of Oral HPV
- There is no cure for HPV but sometimes it disappears spontaneously [4].
- HPV vaccines reduce the risk of getting genital and cervical cancers.
- The vaccines, however, have not been proved to work against oral cancer caused by oral HPV infections [1].
Milia
- These are tiny, hard, white bumps that keep disappearing and recurring [5]
- Mainly occur on the face
- Caused by trapped skin cells that were meant to be shed off [5]
- Common among babies because their oil gland is still developing [6]
- However, it may occur in teens and adults as well.
- Milia have also been attributed to sun damage, lip care products, and reaction to toothpaste.

Image 4 : Infant with milia
Picture Source : skinsight.com
Treatment of milia
- Exfoliation
- Retinol creams [5]
- Do not remove them forcefully since it may cause scarring [6]
Oral thrush
- Caused by fungal infection caused by Candida albicans [1]
- The spots are creamy and may appear on lips, oral cavity, tonsils or the gum
- May be patchy

Picture 5 : Oral candidiasis – White patchy lips
Photo Source : Wikipedia.com
- People using corticosteroids, antibiotics or birth control pills are more vulnerable
- Illnesses such as cancer, diabetes, HIV and anemia compromise immunity and also predispose the patient to the infections [7]
- Pregnancy and organ transplants are also risk factors
Treatment - Antifungal medications [7]
- Can be controlled by managing illnesses such as diabetes properly.
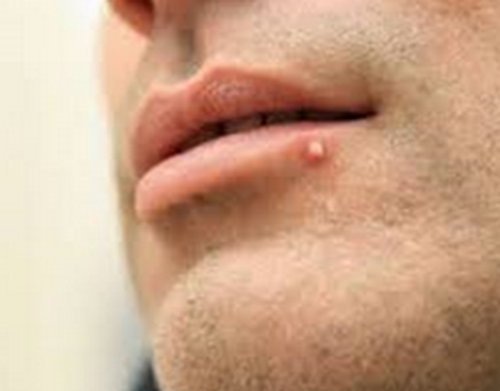
Herpes simplex virus (HSV)
- The spots are painful, white, itchy, and bumpy
- Appear as blisters on the lips
- HSV is contagious and is transmitted through skin contact [1]

Figure 6: Herpes blister on the lower lip
Picture Source: wikipedia
Treatment
- Oral and antiviral medication
White spots caused by oral cancer
- Initially, they appear as white, flat spots on the lip that begin to ulcerate in latter stages.
- The spots then grow, harden and don’t heal

Picture 7 : Lower lip cancerous white bump
Image Source: healcure.org
- Genetics, excessive drinking, smoking, and HPV infections are risk factors [8]
Treatment
- Surgical removal of the tumor, chemotherapy and/or radiation therapy
Canker sores
- These are painful, burning ulcerative patches that are round in shape [9].
- Color ranges from white to gray to pale yellow with red edges

Photo 7 : Canker sores inside lower lip
Picture Source: healcure.org
Causes of Canker sores
- Allergic reactions to elements in food
- Suppressed immune system
- Tissue trauma
- Nutritional deficiencies
- Cohn’s and celiac diseases have also been associated with canker sores [1]
Treatment
- Usually heal with no medication [9].
- In chronic cases a doctor could prescribe antimicrobial mouth rinse, corticosteroid ointment, or OTC [1]
Vitiligo
- Vitiligo is a medical condition in which the melanocytes fail to produce melanin leading to white patches on the skin [10]
- Cause unknown but researchers have linked it with an autoimmune disease, heredity and cancer [1, 9]
- They are more of white patches rather than white spots
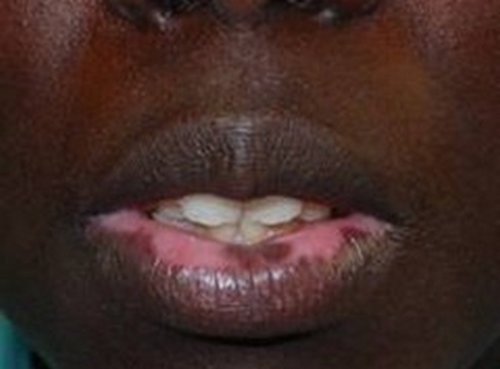
Image 8 : Vitiligo patches on lips
Photo Source: md-health.com
Treatment
- Steroid therapy
- Tattooing
- Skin grafting
- Skin graft
- Melanocyte transplant
- Psoralen photohemotherapy
- Depigmentation
White raised spot due to lip pimple
- A pimple on the lips can cause a white dot on the lip.
Picture 9 : White spot on lip due to pimple
Image Source: pimplestap.com
Treatment
- Varies depending on the cause of the acne
Fibroma
- These are malignant tumors of the connective tissue
- They form from lumps within the mouth
- Attributed to trauma from lip biting and teeth grinding
- Can be pink, or whitish in color

Image 10 : Fibroma white raised spot on inner lip
Photo Source: healcure.com
Treatment
- Surgical removal
Management of White Spots on lips
- Do not scratch the spots on the lips. It could cause an infection [5].
- Rinse the lip with warm and salty water. Swish it then spit
- See a doctor if the spots on the lips bleed, lead to swelling of the neck and jaw, make the tongue numb, or make swallowing difficulty [1, 9].
References :
- Heal Cure. White Spots on Lips Pictures, Small, on Lower, Upper, Inside, Lip Corner Causes Cancer, HPV & Cure [Internet]. 2015 [cited 18 January 2016]. Available from: http://www.healcure.org/lip/lip-bumps-spots/white-spots-on-lips-causes-pictures-small-on-lower-upper-inside-lip/
- Lee J, Lee J, Kwon N, Yu D, Kim G, Park C et al. Clinicopathologic Manifestations of Patients with Fordyce’s Spots. Annals of Dermatology [Internet]. 2012 [cited 18 January 2016];24(1):103. Available from: http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3283840/
- 14. RA M. [Fordyce’s spots: disease, heterotopia or adenoma? Histological and ultrastructural study]. – PubMed – NCBI [Internet]. Ncbi.nlm.nih.gov. 2016 [cited 18 January 2016]. Available from: http://www.ncbi.nlm.nih.gov/pubmed/6943138
- 15. Weiss A, Dym H. Oral lesions caused by human papillomavirus [Internet]. Clinical Advisor. 2011 [cited 18 January 2016]. Available from: http://www.clinicaladvisor.com/cmece-features/oral-lesions-caused-by-human-papillomavirus/article/193918/
- Kunin A. Milia [Internet]. DERMAdoctor Blog. 2012 [cited 18 January 2016]. Available from: http://www.dermadoctor.com/blog/milia/
- Skinsight.com. Milia in an Infant or Baby: Condition, Treatment and Pictures – Overview | skinsight [Internet]. 2016 [cited 18 January 2016]. Available from: http://www.skinsight.com/infant/milia.htm
- Nhs.uk. Oral thrush in adults – NHS Choices [Internet]. 2016 [cited 18 January 2016]. Available from: http://www.nhs.uk/Conditions/Oral-thrush—adults/Pages/Introduction.aspx
- Oralcancer.org. The Oral Cancer Foundation [Internet]. 2016 [cited 18 January 2016]. Available from: http://www.oralcancer.org/
- Md-health.com. White Spots on Lips | MD-Health.com [Internet]. 2016 [cited 18 January 2016]. Available from: http://www.md-health.com/White-Spots-On-Lips.html
- Mayoclinic.org. Vitiligo Causes – Mayo Clinic [Internet]. 2016 [cited 18 January 2016]. Available from: http://www.mayoclinic.org/diseases-conditions/vitiligo/basics/causes/con-20032007




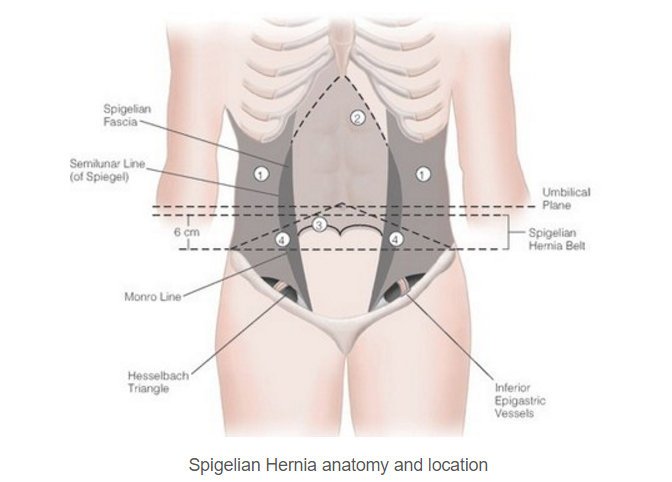 Figure 2 : Shows the position of Spigelian Hernia
Figure 2 : Shows the position of Spigelian Hernia


